This post is part of a series of guest posts on GPS by the graduate students in my Psychopathology course. As part of their work for the course, each student had to demonstrate mastery of the skill of “Educating the Public about Mental Health.” To that end, each student has to prepare two 1,000ish word posts on a particular class of mental disorders.
______________________________________________
For Autism, Treatment is Everything by Jordan Vanderbilt
Autism Spectrum Disorder (ASD) has increased in prevalence over the last 40 years. Experts declare that it is partially explained by the improvements in diagnosis and overall global awareness, while others give less informed opinions. Symptoms of autism are often recognized during the second year of life but may be seen earlier or later depending on the severity. The disorder is portrayed, according to the Diagnostic and Statistical Manual (DSM-5), by deficits in social communication and interaction as well as restricted, repetitive patterns of behavior, interests or activities. Regardless of the cause of the increased frequency, ASD has approached 1% of the worldwide population. With no single known cause as of yet, efforts must be focused on treatment. Unfortunately, a number of states in the U.S. have yet to adopt mandates necessary for some research-supported ASD treatments to be covered by insurance.
There are a number of treatments used to help those with autism, most focusing on specific areas of deficiency. Treatments for ASD are varied and include medications, restricted diets and dietary supplements, therapeutic interventions, and everything in between. At this point there is no single intervention able to combat all of the symptoms and impairments seen in those with ASD. Each of the above interventions can offer results to some degree, however, some are clearly more supported.
 Pharmaceutical companies have fixed their sights on attempting to produce medications to improve comorbid symptoms such as anxiety, hyperactivity, and challenging behavior associated with ASD. The three main families of medication used to treat ASD are antipsychotic medications, serotonin reuptake inhibitors, and psycho-stimulants. Of these three types of medications antipsychotics have shown the most improvement on challenging behavior measured by parent reported hyperactivity. Risperidone and aripiprazole (both antipsychotic medications) have been identified as the two best-studied medications for challenging behavior due to substantial evidence in support of their use and have also shown improvement in other ASD comorbid symptoms. Aripiprazole was rated highest for its effect on challenging and repetitive behavior in comparison to Risperidone’s moderate effects. Unfortunately, both medications were found to cause significant adverse effects such as sedation and weight gain. Another alarming fact about medical intervention resides on the fact that the strongest study results have been funded by pharmaceutical companies who ultimately profit from the treatment.
Pharmaceutical companies have fixed their sights on attempting to produce medications to improve comorbid symptoms such as anxiety, hyperactivity, and challenging behavior associated with ASD. The three main families of medication used to treat ASD are antipsychotic medications, serotonin reuptake inhibitors, and psycho-stimulants. Of these three types of medications antipsychotics have shown the most improvement on challenging behavior measured by parent reported hyperactivity. Risperidone and aripiprazole (both antipsychotic medications) have been identified as the two best-studied medications for challenging behavior due to substantial evidence in support of their use and have also shown improvement in other ASD comorbid symptoms. Aripiprazole was rated highest for its effect on challenging and repetitive behavior in comparison to Risperidone’s moderate effects. Unfortunately, both medications were found to cause significant adverse effects such as sedation and weight gain. Another alarming fact about medical intervention resides on the fact that the strongest study results have been funded by pharmaceutical companies who ultimately profit from the treatment.
For those unwilling to subject themselves or their children to harmful side effects but still want to reduce associated symptoms, many have looked for alternatives of which there are several. GFCF is an acronym for gluten-free, casein-free which refers to a specialized restricted diet that is gaining in popularity with many parents. The theory behind a reduction in gluten and casein suggests that many individuals with autism also show G.I. abnormalities in the ability to break down these substances. Associated symptoms like gastro-esophageal reflux, abdominal pain, and constipation are fairly common in ASD. The literature has not deemed this diet as scientifically valid, many parents nonetheless support it’s use.
One particularly interesting dietary treatment option now being tested is derived from the broccoli plant. Sulforaphane has shown to counteract biochemical and molecular abnormalities in those affected by ASD thus improving behavior. This treatment is a dietary supplement designed to target clinical features as well as biochemical irregularities. Studies show much improved social interaction and abnormal behavior in roughly half of the number of subjects evaluated compared to those who received a placebo.
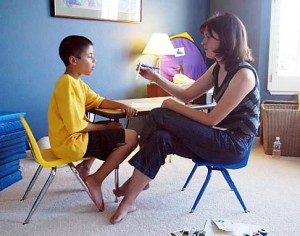
Of the many treatment options available for autism one stands above the rest in terms of evidence-base and effectiveness. Applied Behavioral Analysis (ABA) has become a prominent treatment option not only due to the amount of research support and ongoing data collection but also from its flexibility to be applied at home and at school. ABA offers a wide variety of treatment methodologies that can be tailored to fit the individual. For example, Verbal Behavior Intervention (VBI) uses the principles of ABA, motivates the student to learn language through simple requests (milk) followed by reinforcement (giving them a cup of milk), the word is then used again in a similar context. This type of repetition helps teach that communication can yield positive results. This example is just one of several ABA-based therapies for individuals of any age with autism.
When compared to medications, the side effects of ABA are far less adverse…because there aren’t any. There are also long-term gains seen even after discontinuing formal services, as parents are trained in how to continue using behavioral techniques.
The problem typically associated with ABA therapy for ASD is the cost. Ideally, ABA treatment should be applied for 40 hours per week over at least two years. Now, I’m sure many of you reading this can agree that the cost of something so time-consuming is most likely very expensive. If that is the case, you would do well applying for a job at an insurance company. In all seriousness, initial cost is most likely the reason a number of insurance companies still do not provide ABA therapy. The refusal of coverage is usually based on the premise that is “experimental” or “educational.” What is apparently misunderstood about ABA therapy is that it can be taught to the parents, incorporated into schools, and is essentially a developmental way of life and specific method of learning for individuals with autism.
State mandates requiring insurance to cover ABA therapy are in place in 37 states. Unfortunately, Oklahoma, the state where I was born and raised is not one of them. To add insult to injury Oklahoma is one of five states not currently pursuing autism insurance reform. This news is disconcerting as a native Okie, and most likely, also to anyone touched by ASD currently residing in Alabama, Idaho, North Dakota, and Wyoming.
Ultimately, it is difficult to put a price on a promising therapeutic intervention for the state of Oklahoma because there is apparently no need for it. Alternatively, it is quite easy to put a price on the same intervention per member per month (PMPM) in most of the states with insurance mandates that cover ABA therapy. For example, in 2014 the Maine State Legislature Act to Reform Insurance Coverage to Include Diagnosis for Autism Spectrum Disorders estimated that ABA services would cost $1.48 PMPM or 0.4% of the premium. This amount hardly seems excessive for the critical development of children afflicted with autism.
As mentioned before, ABA therapy is essentially a way of life for individuals and families afflicted with ASD. The only thing restricting this way of life for people in Oklahoma is the policy-makers ability to be forthright and willing to help this growing population achieve the same quality of life as any other Oklahoman.